SONHP Professor Wins Award From the California Association for Nurse Practitioners

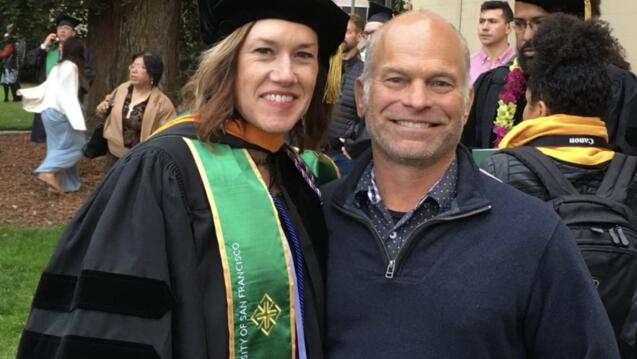
USF’s Alexa Colgrove Curtis PhD, MPH, FNP, PMHNP received the Bridging Health Care Needs Award from the California Association for Nurse Practitioners (CANP).
In an interview with CANP, Curtis — assistant dean of graduate nursing, professor, MPH-DNP dual degree director, and co-chair of the CANP Health Policy and Practice Committee — said that she has always focused on youth and rural communities.
In the last four years, she collaborated with an interprofessional team to start a treatment center in a rural area to treat opioid use disorders and other addictions.
As a professor at the USF School of Nursing and Health Professions, she focuses on developing a workforce for underserved, rural communities, particularly to address substance use disorders.
Under an HRSA grant, she is working to increase the number of nurse practitioners in rural communities, with abilities to undertake mental health, substance use disorders, and other health matters such as childhood obesity and telehealth.
Curtis has also led some global work. She helped to open the Uganda Nurse School in Bwindi and has facilitated USF learners to work with the Bwindi team to improve access to care and lead bi-directional learning.
Most recently, in collaboration with La Ibero-Americana in Tijuana, Curtis and USF DNP students will do a similar shared learning program to prepare both groups of nurses to meet the needs of migrants in California.
When asked about the National Academies of Sciences, Engineering, and Medicine’s new report, “The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity,” Curtis spoke about how the report affirms how communities are better served when nurse practitioners work without practice barriers and that the quality of care nurse practitioners provide is equal to that of interprofessional colleagues and, in some cases, better.
“There are barriers to anything you want to do that is meaningful and innovative. We are framing barriers as challenges that can be handled with collaboration and persistence,” said Curtis.
Curtis emphasized how nurse practitioners want to fill in the health care gaps across communities. For her, nurses are natural advocates anyway. They are taught from day one in nursing school that they are their patient’s advocates. Then, their advocacy expands to populations, particularly when it concerns underserved populations.
For Curtis, if you want to be an advocate for the community, you have to become involved in political advocacy and move policies forward, such as AB 890 (Wood), that can unleash the potential of nursing and nurse practitioners to bridge the health care needs of communities, she said. In 2020, CANP and its members achieved a monumental victory with the passage of AB 890, legislation that allows nurse practitioners to practice without physician supervision in California. The organization is now working to implement the bill.
“CANP supports nurse practitioners to move the profession forward and meet the health care needs of their communities,” said Curtis. “It has just been a tremendous honor to be a nurse and a nurse who also works in academia.”
Full Interview
Please briefly describe your areas of expertise and the work you are leading as a nurse practitioner to address:
- Rural and youth health
- Substance use disorder prevention and treatment
- Workforce development and
- Global health partnerships
All the things I do intersect in different ways. I started my nursing journey as an acute care pediatrics nurse and transitioned into primary care focusing on youth. My master’s work was with pregnant and parenting adolescents, and since I have continued with a youth focus within rural communities. My initial work as a nurse practitioner was in extremely remote populations. My husband was in the military, and I worked in the remote community of Needles, California to provide family care services to an underserved population. After this experience, I went from the high desert to the Sierra Nevadas, where I collaborated on the development of a school-based health center for pregnant adolescents at a rural alternative high school and helped to start the first junior college student health services at our satellite campus in the community. Then my PhD at UCSF focused on rural health and youth and I became a member of the Leadership in Education for Adolescent Health. In the last four years, I collaborated on the development of a Medication Assisted Treatment Center (MAT) in a rural community. MAT is a pharmacological and behavioral health therapy to treat opioid use disorders and other addictions.
As faculty at the University of San Francisco, most of my work has been on developing the workforce for underserved, rural communities, particularly in the areas of substance use disorder. Under a current HRSA grant, we are working to increase the pipeline of nurse practitioners providers in the rural community, particularly with abilities to address mental health, substance use disorders, and other health matters such as childhood obesity and implementing telehealth. With a previous SAMHSA grant, I worked on ensuring our nurse practitioners — including at USF, UCSF, and Sonoma State — completed their programs with the ability to manage opioid use disorders. Then in my free time, I’ve been able to do some global work. I have worked on helping to open the Uganda Nurse School in Bwindi and have facilitated USF learners to work with the Bwindi team to improve access to care and lead bi-directional learning. Most recently with a collaboration with La Ibero-Americana in Tijuana, we will do a similar shared learning. We will focus on how we better prepare both groups of nurses to meet the needs of migrants in California.
The National Academies of Sciences, Engineering, and Medicine released “The Future of Nursing 2020-2030: Charting a Path to Achieve Health Equity” report. Can you comment on a few key highlights of this report as it impacts your work and the CANP goals?
Highlighted in the 2010 Future of Nursing Institute of Medicine (IOM) report is that: 1) nurses needed to be full partners in the redesign of health care delivery to meet the needs of the communities; 2) academia needed to double the doctorally prepared nurses, which has happened with the help of doctor of nursing practice programs like the one we have at USF and others across California; 3) in order to meet the community’s health care needs, IOM recommended to remove practice barriers to care for nurses. That was 2010. Now fast forward to 2020-2030. The IOM, now the National Academies of Sciences, Engineering, and Medicine, released an interprofessional report. And what is their recommendation? To remove barriers to practice for nurse practitioners so that all nurses work at the full scope of their education and training. The report highlights that the data consistently affirms that communities are better served when nurse practitioners are working without practice barriers. The report also highlights that the quality of care nurse practitioners provide is equal to that of our interprofessional colleagues and, in some cases, surpassed the effectiveness. So artificial barriers to practice for nurse practitioners are holding back the health of the community. In the United States, we continue to have more states with full practice authority of practice for nurse practitioners. That means nurse practitioners are not obligated to have physician’s supervision in order to practice as nurse practitioners. The last state that granted full practice authority was Massachusetts in January 2021. Nurse practitioners continue to gain ground in full practice authority and through the efforts of the CANP and in collaboration with the bill author, Assemblymember Wood, we were able to finally, after years of efforts, get a bill passed in California that has a pathway to independent practice for nurse practitioners. The bill is AB 890, and it was a full-court press for the entire nurse practitioner community, many of our interdisciplinary health colleagues and organizations. We are thrilled to do our part as California tries to meet the objectives of the Future of Nursing report in terms of removing practice barriers in nurse practitioners’ practice.
The 2020-2030 Future of Nursing report also highlights that nurse practitioners are essential to addressing our health inequities, both racial/ethnic and geographic. The Future of Nursing report looks at increasing care of rural communities, other underserved populations, mental health, substance use disorders, maternal health, and caring for our older adult population. These are all things that are absolutely in the nurse practitioner’s wheelhouse. We are excited as nurse practitioners to move forward and meet the health needs of communities.
Now that the AB 890 passed and was signed by the governor, we are working with the stakeholders, particularly the Board of Registered Nurses, to get the implementation and regulations written and in place. Nearly half of the U.S. states and territories have full authority for nurse practitioners and California had not moved in that direction until the last legislative session.
How do you describe the role of a nurse practitioner to provide care to their patients, particularly in rural areas?
The role as a nurse practitioner might not be that different. I am providing health care, behavioral health, and substance use disorders services. What can happen with the implementation of the AB 890 is that nurse practitioners will set up a practice to address the niches that have not been filled and meet the health care needs of an underserved population. As an example, there is another bill currently in the legislature to give immediate authorization to have Medical funding for homeless populations. If a nurse team encounters a homeless population, they would be able to provide care and bill Medi-Cal for those services under presumptuous authorization. That is incredible practice! It is a street nursing practice where you can actually care for the homeless in a sustainable way. There is a plethora of other very creative practices that nurse practitioners could perform if they were able to open a practice without all of the red tape, without having to find and pay a supervising physician. In many of these underserved areas, there is no supervising physician available, so it just stops access to care, plus it adds cost. The Veterans Administration (VA) removed practice barriers for nurse practitioners throughout the VA, and it has lowered the bureaucratic costs as you hire a nurse practitioner and let them practice.
As a catalyst for positive change in the health care system, what are some of the key learnings you’ve had to continue to make progress?
There are barriers to anything you want to do that is meaningful and innovative. We are framing barriers as challenges that can be handled with collaboration and persistence. Staying mission-centered to the driver of being a nurse and care for people and populations, we are doing extremely meaningful and needed work. However, while being mission-centered, we also have to be margin and policy-savvy. Our academic systems, both the master’s and doctoral programs, are teaching nurses to be expert nurses and provide medical care within the nursing framework. But they also need to know how to move a business forward, organizations forward, how to move policy forward. If we don’t do that, we just continue in the same box as people capable of doing great work without the latitude to actualize our potential as a profession.
In your practice, you are definitely “bridging health care needs.” Is there a conceptual model that guides your work?
As a nurse and a nurse practitioner who has primarily worked in rural communities, I operate from the social-ecological model. This model looks first into the intrapersonal forces, what is specific to the individual; then the interpersonal influences, what is going on within the client’s immediate interactions. Then look into the organizational influences, the possibilities, and the structural barriers to care within organizations. Then moving forward into the community, what is the surrounding community, what are those forces that are going to look different. Providing care is different in each rural community, and it certainly looks different in a rural community in California versus in Uganda. Then looking into the larger sphere, the policy realm. At an international/national level, what policy is shaping our ability to provide health care for that individual and that population that we serve?
Then within my work with youth, I work from the development theory and contextualism that looks at human beings’ development in a context within the life span theory. This life span theory includes concepts of plasticity, which is our ability to change throughout our life span, recognizing people and populations have the ability to change. And the approach also looks into their reserved capacity to meet challenging situations and then, of course, working with youth, concepts of resilience. How do they accommodate the challenges they encounter and internalize the benefits and opportunities to actualize their potential.
How does your nursing practice, work in academia, and CANP advocacy leadership intersect? How does this intersection inform your impact?
At the heart of my being, I am a nurse, and that is where it all starts. Because I am a nurse and committed to serving underserved populations, I always want to know how to be effective and then be more effective. That is why the academic perspective is essential. I love being a nurse; therefore, I love studying nursing, love investigating how to do even better work with more significant impact. The other part of being an academic certainly is the raising up of the next generation of advanced practice nurse leaders, nurse practitioner leaders. It is such an amazing opportunity to work with the nurses stepping up and coming forward. Nurse practitioners are not generally coming into the profession because they want more money or fame. In fact, many nurse practitioners might make less money than those working in an acute setting. Nurse practitioners are truly mission-centered and want to meet a need and address the gaps in the community. It is inspiring to work with future leaders in health care.
Going back to that social-ecological model, you need to become an advocate. Nurses are natural advocates anyway; that is, what we are taught from day one in nursing, you are your patient’s advocate. Then that expands to be an advocate for a population and particularly an underserved population. You are an advocate for the community and understand you have to become involved in political advocacy to move policies forward, such as the AB 890 that can unleash the potential of nursing and nurse practitioners to meet the health needs of communities.
When a patient says, “You saved my life,” you realize the impact that goes underappreciated. Nurse practitioners save lives day-to-day in underserved communities by providing that relationship, patient-centered, high-touch, holistic, expert medical care within the nursing framework.
What would you tell your students is most important about engaging in advocacy efforts on behalf of the nurse practitioner community and profession? Why does it matter? How has it impacted your own career?
Advocacy is part of nursing 101. We work with students to develop the skills and capacity to go out and be advocates on a broader scale in the community and the policy arena — faculty models with our advocacy. I often talk with students about my work on the AB 890. We encourage students to become engaged in the local CANP chapters, and we encourage our students to become involved at the state-level organizations. We bring them on as partners with us in this journey to push the nurse practitioner profession forward.
CANP supports nurse practitioners to move the profession forward and meet the health care needs of their communities. It has just been a tremendous honor to be a nurse and a nurse who also works in academia. And it has been an honor, a pleasure, and a memorable experience to participate on the board of the CANP to help move our profession forward.
About the California Association for Nurse Practitioners
The California Association for Nurse Practitioners is the unifying voice and networking forum for nurse practitioners, providing guidance and advancing the nurse practitioner profession statewide.
About the Bridging Health Care Needs Award
The California Association for Nurse Practitioners Bridging Health Care Needs Award recognizes nurse practitioners who are active as a catalyst for positive change in the health care system, and who demonstrate the value of the care nurse practitioners provide to their patients.